Urolithin A is produced from the breakdown of ellagic acid, which is high in foods like berries, nuts, pomegranate and is classed as a post-biotic. Its likely to be a significant contributor to the anti-cancer effects of tree nuts (see Walnuts in the Foods Library). Only about 40% of adults over 50 produce urolithin A from dietary sources, and this declines with age partly due to poor microbiome diversity.
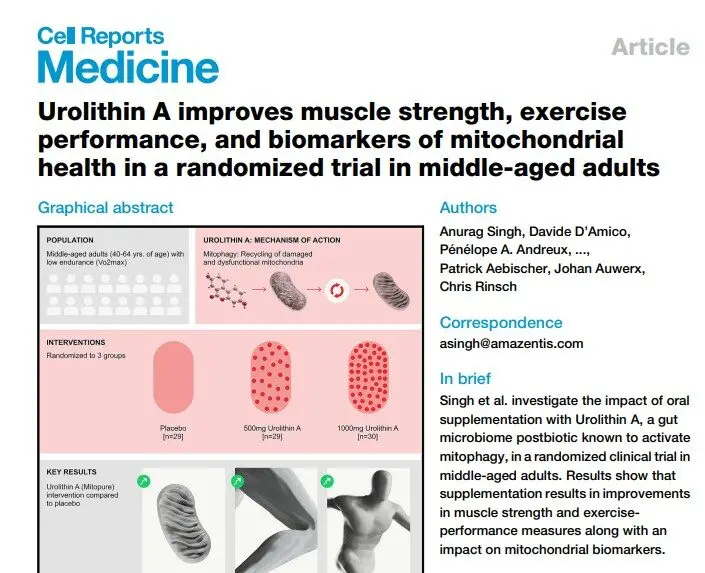
With the emergence of the mitochondrial theory of cancer, this compound is gaining attention due to its ability to stimulate called mitophagy, or renewal of mitochondria the “engines” of cells. Mitochondrial dysfuntion is clearly and significantly seen in cancer, and is already verified as a dominant marker of glioblastoma, lung, colorectal and ovarian cancers. Importantly, urolithin A can suppress acylcarnitines, compounds that play a pivotal role in regulating lipid and sugar metabolism. High levels are linked closely with progression in several cancers including glioma, liver, prostate and breast cancer, . In kidney cancer, research shows 3 to 6X increases in these molecules in the tumor environment, and resulting upregulated fatty acid availabliity drives progression – high levels and are proposed as biomarkers for the disease. Studies in anti-aging find strongest effects at 500mg dose.
One study showed only 12% of adults around 50 had circulating levels of urolithin a and with that, they had good levels of key gut bactiera including Akkermansia muciniphilia. These bacteria play a crucial role in successful immunotherapy. There is a large volume of pre-clinical data in cancer research for urolithin A, and one result is the recent initiation of a multi-center phase II trial in early phase prostate cancer to establish its overall suitability (see References)
Pilot show systemic effects of urolithin A, noting significant anti-inflammatory actions in overweight adults, reducing c-reactive protein and IL-beta. 500 and 1000mg doses were used without any side effects and good absorption (highlight 1). Nestle is in trials of branded Mitopure for anti-aging.