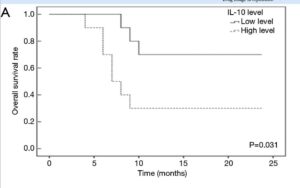
Fascinating pilot study looking at curcumin + piperine (black pepper) at 8 x 500mg daily along with 500mn taurine in the progression of late stage liver cancer patients. The analysis confirmed beneficial suppression of IL-10 inflammatory markers and regulation of so called microRNA molecules that regulate gene expression affecting progression rates, including reduced effecs of oncology drugs.
Whilst this is a small scale investigation, the results both confirmed significant effects of the combined natural compounds, and most remarkably the overall survival times were almost doubled in those with low miR-21 levels as a result of the strong suppression effects of the 3 ingredient supplement regime:

MicroRNAs are small RNA molecules with activity that changes gene expression. Small changes in microRNAs can occur inside the tumor cells, making them resistant to chemotherapeutic agents. Relatively high levels of miR-21 substantially reduce relative survival in HCC patients especially after surgical resection:
https://www.spandidos-publications.com/10.3892/mco.2018.1603